To date, close to 180,000 cases of the novel coronavirus have been reported worldwide with over 7,000 fatalities. After days of uneasy calm, Ghana has, rather sadly, recorded its first six cases of the deadly disease. As much as we hope that no more cases are recorded, the likelihood that this number will grow in the coming weeks is high. This has resulted in government putting in place measures aimed at checking the spread of the virus. Once our prisons are an extension of society, it is necessary for all actors in this fight, to as a matter of urgency, map out strategies to prevent the deadly virus from entering our facilities and prepare also for the worst.
Overcrowded and poorly ventilated cells
With an overcrowding rate hovering around fifty percent, most of our prisons present fertile grounds for the spread of diseases. The continuous admission of newly convicted persons and the competition for sleeping space in facilities result in prisoners bunching up on floors of cells, eliminating the opportunity to practice social distancing, thereby creating conditions for the spread of the COVID-19 virus.
Our facilities have endured outbreaks of scabies, tuberculosis, hepatitis and in 2018, the H1N1 influenza. The outbreak at Ankaful Maximum Security Prison resulted in about 300 prisoners as well as about 100 officers and their dependents suffering from the H1N1 influenza.
Though protocols to prevent the spread of communicable diseases are activated whenever required, overcrowding renders the efforts somewhat counterproductive.
Most of Ghana’s prisons are remnants of the colonial era such as forts, castles and armouries. Such facilities are not purpose-built and so do not offer environments that support healthy living. They are mostly not properly aerated and or illuminated allowing easy transmission of diseases. Despite attempts by the prison administration over the years to modify these structures and make them more habitable, outbreaks of communicable diseases over the years suggest that, there is the need to invest in building requisite structures to support the wellbeing of prisoners, prison staff and visitors.
Visits
Visits to prisoners form part of the service’s drive to encourage continuous family support to the incarcerated. Prisoners are allowed a visit every other week but enjoy unfettered access to lawyers and medical doctors according to prison regulations.
Prisoner visits by friends and families have become topical as there are increasing fears that visitors and or prison staff may pass on the disease to prisoners. Italy is the first country since the outbreak to ban face-to-face visits from friends and families of the incarcerated. The act led to unrest across the country’s prisons which resulted in over 12 deaths as prisoners rioted against the measure. Countries like Kuwait, Kenya, Jordan, Czech Republic, Philippines and a host of others have since followed suit. The measure by these countries probably is the result of Iran’s decision to release some 70,000 prisoners on furlough following some deaths associated with the outbreak.
How prepared are our prisons?
The prison system in Ghana has existing protocols in place to manage outbreaks of infectious diseases. These include screening of prisoners and all persons who enter prisons, provision of sanitizers and running water for use at the gate and vantage points inside prisons, wearing of face masks by prison staff and visitors, quarantining and referral of suspected cases to appropriate health facilities among others.
Despite the above efforts, the Service is undoubtedly challenged due to the negative effects of overcrowding in our prisons. Basic necessities like water and ablution facilities which support hygienic living are overly stretched. The Nsawam Medium Security Prison, for example, has about 3,500 prisoners sharing facilities originally meant for about 790 people.
Apart from the Nsawam Medium, Ankaful and Koforidua prisons which have relatively more resourced health facilities, most of our prisons operate near-empty infirmaries, incapacitating them from sufficiently catering for prisoners’ health needs. Some prisons lack infirmaries altogether and so depend on limited drugs kept in first aid boxes. It is obvious from the above picture that, most of Ghana’s 44 prisons would be hard hit in the event of any deadly outbreak like the COVID-19.
Improving conditions
Prison conditions such as overcrowding, poor ventilation, poor nutrition and inaccessible healthcare are the major causes of diseases behind bars. A conscious effort should be made to improve on the deplorable state of our facilities. With the creation of new regions, it would be appropriate for government and corporate Ghana to invest in the construction of prisons in these new regions to help decongest the 44 existing facilities. This will help improve prison conditions to an extent and reduce the spread of communicable diseases in the process.
There is the need to look beyond the crimes committed by the incarcerated by accepting that prison health is public health. Effective communication and coordination should exist among all actors in the healthcare space to ensure that healthcare delivery in prisons is integrated into national health policies and addressed as a public health issue.
Infirmaries and clinics in our prisons should be considered in the disbursement of the $100m provided by government to enhance the country’s coronavirus preparedness and fight. Prison health facilities require expansion, materials and equipment to meet the needs of our over 15,000 prisoners as well as officers and visitors to our facilities.
It is necessary to note, as Anthony M. Kennedy, a former American Supreme Court Judge, rightly said, “A prison that deprives prisoners of basic sustenance, including adequate medical care, is incompatible with the concept of human dignity and has no place in civilized society”.
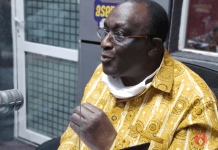
DSP. DANIEL MACHATOR
DEPUTY CHIEF PUBLIC RELATIONS OFFICER
GHANA PRISONS SERVICE
[email protected]